Semen Analysis
How is a Semen Analysis Interpreted?
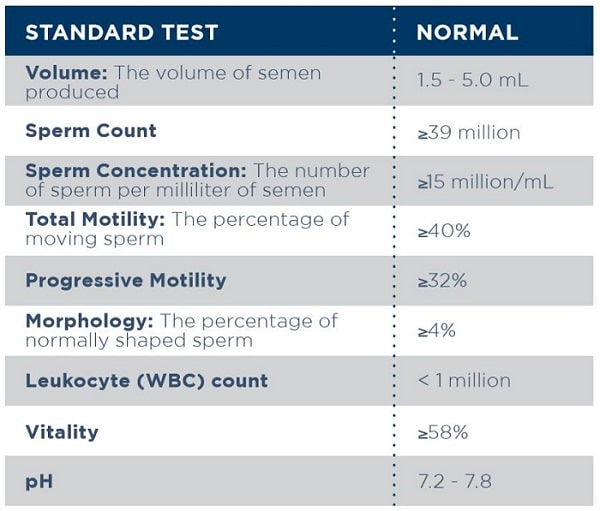
A semen analysis is one of the main tests that a reproductive urologist will use to evaluate your fertility. Interpretation of results may vary from one lab to another because there are several different methods by which sperm can be evaluated. Additionally, each sample that a patient provides will be different due to normal variation and other factors, such as the abstinence period, comfort level, and time and location of the produced sample. This is why any abnormal findings need to be confirmed with at least 1 additional semen analysis. Men with abnormal semen parameters should undergo a comprehensive evaluation, including a history, physical examination, and blood tests to check for hormone abnormalities. Even with an abnormal semen analysis, most men can father children.
Semen Analysis Evaluation
A normal range is provided, but infertility is not known to have any association with an abnormal semen volume. However, efficient delivery of semen to the female during intercourse can be compromised by unusually low or high volumes. Usually, a low volume of semen is an indication of an obstruction or an incomplete collection.
Sperm is quantified in two ways: total count and concentration (sperm/mL). Although a low sperm count often is associated with infertility, some men with low sperm counts can conceive naturally. Low sperm concentration can be caused by hormonal, environmental, anatomic, and genetic factors.
Some labs will rate the quality of sperm motility using a grading system. The percentage of sperm which have forward, or progressive, motility is an important value. There are several possible causes of low motility, including sperm antibodies, leukocytospermia (white blood cells in semen), infection, and varicoceles.
An egg (oocyte) from the female has the best chance of being fertilized by morphologically normal sperm. Most sperm have a morphologic abnormality. When couples undergo IVF, the sperm will be evaluated carefully so that normal sperm are used.
Normozoospermia: All semen parameters are within normal limits
Oligozoospermia: Sperm concentration is <15 million/mL
Azoospermia: No sperm detectable in the ejaculate
Aspermia or hypospermia: No ejaculate or low volume ejaculate
Asthenozoospermia: Percentage of moving sperm <40%
Teratozoospermia: Percentage of morphologically normal sperm <4%
Oligoasthenoteratozoospermia: Abnormalities in concentration, motility, and morphology
Leukocytospermia: Number of WBCs in semen is ≥1 million
