Varicocele
What Is a Varicocele?
If you have never heard of the word “varicocele,” you’re not alone. While the term may not come up in everyday conversation all that often, it is one of the most common issues adult men experience (whether they know it or not). In fact, at least 15% of all men have a varicocele. So, what is it, and how worried should you be about it?
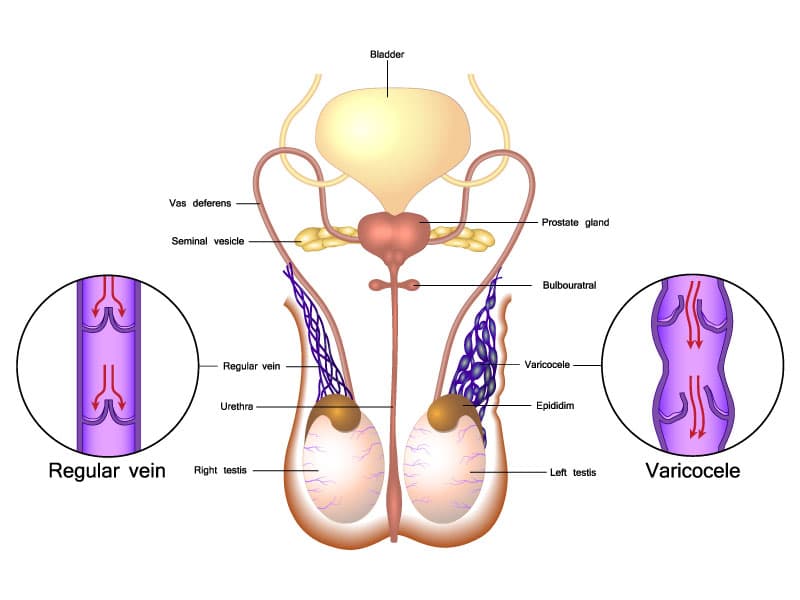
A varicocele is the abnormal swelling or dilation of varicose veins around a testicle. Since these veins transport oxygen-depleted blood out of the testicles and back toward the heart, this swelling means that the blood pools in the veins instead due to malfunctioning valves. The good news? A varicocele is usually not dangerous or life-threatening. As it often doesn’t cause any symptoms or problems, a varicocele can go unnoticed, undiagnosed, and/or untreated without serious ramifications. However, in certain situations, delaying or forgoing treatment can have consequences.
Varicocele Frequently Asked Questions
If you’re experiencing any of the above symptoms, it’s important to make an appointment with your doctor. Your healthcare provider—typically a urologist—can diagnose a varicocele by physical examination, and they will likely assess your scrotum when you’re both standing up and lying down. To assist in their evaluation, your doctor may use the Valsalva maneuver, a technique that involves you taking a deep breath, holding it, and bearing down. This can help your doctor more easily see and inspect the varicocele.
In addition, your healthcare provider may also perform an ultrasound. This painless imaging exam can confirm the presence of a varicocele, rule out other potential causes of your symptoms, and/or identify any other factors contributing to your symptoms.
Treatment for varicocele should be considered for men with pain in the scrotum and/or infertility and an abnormal semen analysis. Varicoceles are treated with an outpatient surgical procedure under general anesthesia. The surgery takes approximately 30-45 minutes per side. In a varicocelectomy, a small groin incision is made and a surgical microscope is used to identify the dilated veins within the spermatic cord, a structure which carries blood vessels, nerves, and the vas deferens to the testicles. The dilated veins are tied off and cut.
Serious complications of varicocele repair are rare. Risks include pain/swelling, bleeding, infection, injury to the testicles, and the risks of general anesthesia. Persistence or recurrence of varicocele after surgery occurs in about 10% of patients. Following surgery, a majority of men will see an improvement in their semen parameters in about 3 months.
Most men will take 1-2 days off work and experience mild pain/discomfort at the incisions and in the scrotum for 1-2 weeks. The pain can usually be managed with ice packs and over-the-counter medications. Patients are asked to refrain from heavy lifting, exercise, and sexual activity for 1-2 weeks.
For some men, a varicocele can be tied to testicular atrophy (shrinkage), infertility, low testosterone, and scrotal pain. If left untreated, a varicocele may:
- Cause the affected testicle to shrink. Due to the malfunctioning valves in the veins in the affected testicle, blood is unable to circulate efficiently and pools in the veins instead. This pooling of blood increases the pressure around the testicle, which may cause the testicle to shrink ultimately due to tissue loss.
- Negatively impact fertility. The pooling of blood in the affected testicle can raise the temperature of the scrotum. Over time, this increase in temperature can damage the number, quality, and motility of sperm, leading to fertility issues.
- Result in low testosterone levels. Varicoceles can damage the cells in the testicles that produce testosterone. Low levels of this essential hormone can lead to a reduced sex drive, the inability to get or maintain an erection, feeling tired all the time, and the loss of lean muscle mass, among other symptoms.
- Cause chronic pain. The excess pressure in the affected testicle may produce discomfort or dull, aching pain in the scrotum that can range from mild to severe. Pain is often more noticeable or intense later in the day or after prolonged periods of standing since gravity can increase the pressure felt from the blood pooling in the affected varicocele.
Treating or surgically repairing the varicocele can help address these complications, relieve any associated symptoms, and improve your quality of life.
Varicoceles more often occur in the left testicle or both testicles due to how the veins in the body are connected. In about 15% of cases, a varicocele can develop solely in the right testicle. An isolated right varicocele may indicate the presence of a mass or blockage in your abdomen, which may require surgery or other treatment to resolve successfully. That’s why if you have a varicocele, you must discuss with your doctor whether repairing it is right for you.
The reason why men can develop varicoceles is unknown. While weakening valves within veins can be related to getting older, varicoceles can also form during puberty and develop over time.
Not all cases of varicoceles cause discomfort, pain, or other symptoms, so many men are unaware they even have one and don’t experience any adverse side effects. However, possible symptoms include the following:
- Blood pooling in the testicle can cause dull, aching pain or discomfort in the scrotum. These sensations are typically more pronounced later in the day or when standing. Lying down often relieves the pain, as gravity no longer creates excess pressure in the scrotum.
- A mass in the scrotum. If a varicocele is large enough, a mass that resembles a “bag of worms” may be seen above the affected testicle. Similar to varicose veins found in the legs, the “worms” are the swollen veins around the testicle.
- Testicles of different sizes. The affected testicle (usually the left) may be markedly smaller than the other.
- A varicocele can negatively affect sperm count, quality, and motility. This may lead to difficulty conceiving a child—for the first time or subsequent children.
The varicocele grading system characterizes the size of the varicocele and can help determine the best course of treatment if needed:
- Grade O: The varicocele can’t be physically felt by you or your doctor but can be seen on an ultrasound. This is often called a subclinical varicocele.
- Grade I: Your doctor can physically feel your varicocele when you perform the Valsalva maneuver during your exam.
- Grade II: Your doctor can physically feel your varicocele without needing to use the Valsalva technique.
- Grade III: The varicocele is visible to the naked eye and may have changed the look or shape of your scrotum.
Since varicoceles may not cause any signs or symptoms, some men don’t know they have one until they experience fertility problems. Of the 15% of couples in the U.S. who have trouble conceiving, male infertility plays a role in approximately 50% of the cases. Male infertility can be due to several factors, such as low sperm count, often caused by varicoceles.
Varicoceles are the most commonly identified cause of male infertility worldwide—up to 40% of men with male infertility have varicoceles. For men experiencing secondary infertility (difficulty conceiving subsequent children after successfully conceiving children in the past), a varicocele may be the culprit up to 70% of the time.
It’s important to note that a varicocele doesn’t necessarily, or always, contribute to male infertility. In fact, about 80% of men with varicoceles can conceive children without requiring intervention. However, since a varicocele can impact sperm production and motility, it’s possible that if you’re experiencing trouble conceiving, you may be diagnosed with a varicocele while being evaluated for infertility.
The scrotum hangs below the body because the temperature of the testicles needs to be cooler than the inside of the body. When the veins in the affected testicle become enlarged due to malfunctioning valves, the temperature in the scrotum can increase. This increase in temperature can “overheat” both testicles in the scrotum and decrease the number, motility, and quality of sperm produced, decreasing fertility.
Testosterone is primarily produced in the testicles, and men with varicoceles often have lower testosterone levels than men without varicoceles. Experts suggest that varicoceles may impair the cells that produce testosterone, indicating a link between varicoceles and hormonal dysfunction.
If left untreated, it’s possible that over time a varicocele could grow in size, cause further decline in testicular function, further impair fertility, or cause pain. You are also more likely to develop a varicocele as you get older due to the weakening of vein walls that tends to occur with age.
It may be comforting to know that varicoceles do not typically rupture. In the unlikely event that it does happen, a sudden increase in abdominal pressure, leading to increased pressure in the testicular veins, could cause varicocele veins to burst. Symptoms may mimic testicular torsion and could include swelling and sudden and consistent pain that is severe. If you experience these symptoms, seek medical attention immediately. But again, varicocele veins rarely burst, so this is likely nothing you need to worry about!
It may—becoming aroused, having sex, and ejaculating can cause physiological changes to your varicocele, so it’s important to understand how sex impacts it. First of all, having sex naturally increases the volume of blood to the testicles—in men with a varicocele, this extra blood flow increases the amount of blood pooling in the varicocele veins. This increase in blood pooling can further damage the affected veins as well as the testicles by increasing inflammation and raising the temperature of the testicles. The rubbing and tugging that can occur during sex can also increase inflammation in the varicocele. The end result is that the overall temperature increase and inflammation can impair sperm production, further weaken the walls of varicocele veins, and decrease testicular function.
Now for some good news—many men with varicoceles have sex without experiencing significant problems. If you have a varicocele, speak with your doctor about how sex could potentially impact your varicocele and what steps you can take to mitigate any risks.
Many men with varicoceles have normal erectile function. However, varicoceles can impact testosterone production, and men with varicoceles are more likely to have lower testosterone levels. One symptom of low testosterone is an inability to get an erection, so if you’re having trouble getting hard, check with your doctor to see if you have a varicocele.
It’s possible—when blood pools in the varicocele veins, it causes inflammation and increases the temperature of the testicles. Since the testicles need to be cooler than the inside of the body, the body can respond to this “overheating” by dropping the testicles lower to prevent them from getting too hot.
Yes, it is perfectly safe to take erectile dysfunction medications if you have a varicocele.
Most men can resume sexual activity about 2 weeks after surgical repair. However, it will take three to six months for any noticeable improvement in sperm count and quality. Suppose you undergo treatment for your varicocele to improve your fertility. In that case, your doctor can give you a timeline for when you should expect to see a potential improvement in your efforts to conceive with your partner. Not everyone who undergoes varicocele repair will have improvement in their sperm parameters.
